Silicone Pulmonary Embolism: A Case Report
-

-
JL
José Arnulfo López-Pulgarin, n/a
Dr. José Arnulfo López Pulgarin, Critical Care and Internal Medicine
Hospital Civil de Guadalajara "Fray Antonio Alcalde"
Guadalajara, Jalisco, MexicoDisclosure information not submitted.
-
GA
Guadalupe Aguirre-Avalos
Dr.
Hospital Civil De Guadalajara, United StatesDisclosure information not submitted.
-
Luis Enrique Colunga-Lozano
Dr. Luis Enrique Colunga Lozano, Internal Medicine and Critical Care
Hospital Civil de Guadalajara "Fray Antonio Alcalde"
Guadalajara, Jalisco, MexicoDisclosure information not submitted.
-
.jpg)
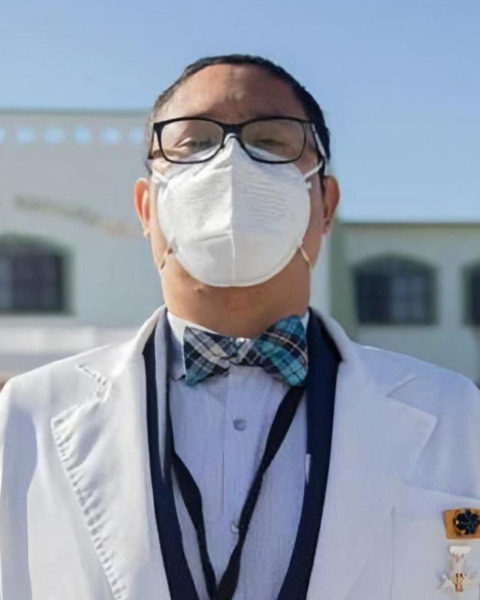
Miguel Ibarra-Estrada, MD
Dr
Universidad De GuadalajaraTax ID: UGU250907MH5
Guadalajara, MexicoDisclosure information not submitted.
-
QC
Quetzalcoatl Chavez-Peña
Dr.
Hospital Civil Fray Antonio Alcalde, United StatesDisclosure information not submitted.
-

Julio Mijangos-Mendez, MD
STAFF
Hospital Civil Fray Antonio Alcalde
Zapopan, Jalsco, MexicoDisclosure information not submitted.
-
.jpg)
Meghan Breed, MD
Vanderbilt University Medical Center
Nashville, TennesseeDisclosure information not submitted.
First Author(s)
Co-Author(s)
Title: SILICONE PULMONARY EMBOLISM (SPE). CASE REPORT.
Case Report Body:
Introduction: SPE is a rare entity reported in medical literature. Clandestine silicone application has been increasing in Mexico, leading to increased rates of SPE and death. Symptoms include dyspnea, chest pain, fever, cough, diffuse alveolar hemorrhage (DAH), and acute respiratory distress syndrome. In Mexico, from 2005-2014, 21.8% SPE deaths have been reported related to cosmetic procedures.
Description: A 21-year-old, previously healthy transgender patient, with a history of multiple cosmetic surgeries, underwent to a gluteal augmentation procedure through injection of 1000 cc of liquid silicone in an outpatient clinic. The procedure was canceled after administration of 500 cc of silicone due to dyspnea and cough, and the patient was discharged. Two days later, the symptoms worsened, and she was admitted to the emergency department, with a blood pressure of 90/64 mmHg, SpO2 60%, respiratory rate of 40 bpm, and heart rate of 125 bpm. She was intubated and admitted to ICU. On clinical examination, we identified basal crackles, petechial hemorrhage, and erythematous puncture sites. CT pulmonary angiogram showed bilateral basal ground-glass opacities, ruling out thrombus in pulmonary circulation; and lung ultrasound with B pattern. Blood test showed thrombocytopenia, hypoxia (Pa02:FiO2 97 mmHg), elevated alveolar-arterial gradient, negative PCR SARS-CoV-2, and no renal failure. She was diagnosed with SPE; supportive management with lung protective ventilation, prone positioning (PP) and systemic steroids (SS) was initiated. She also had hemoptysis, new pulmonary infiltrates, and abnormal liver enzymes at ICU, which resolved spontaneously. After 8 sessions of PP, oxygenation improved, tracheostomy was performed due to ICU acquired weakness and was discharged home after 20 days of hospital stay.
Discussion: There is a paucity of reports of this complication. Our patient showed a significant improvement after administration of SS, which consists with an immuno-mediated mechanism. Studies have reported mortality from 24 to 33%, but can reach up to 100% if neurological symptoms are present. It is important to recognize that silicone injections are not safe and can lead to serious complications. Recognizing rare manifestations can help to distinguish this entity from other etiologies.
